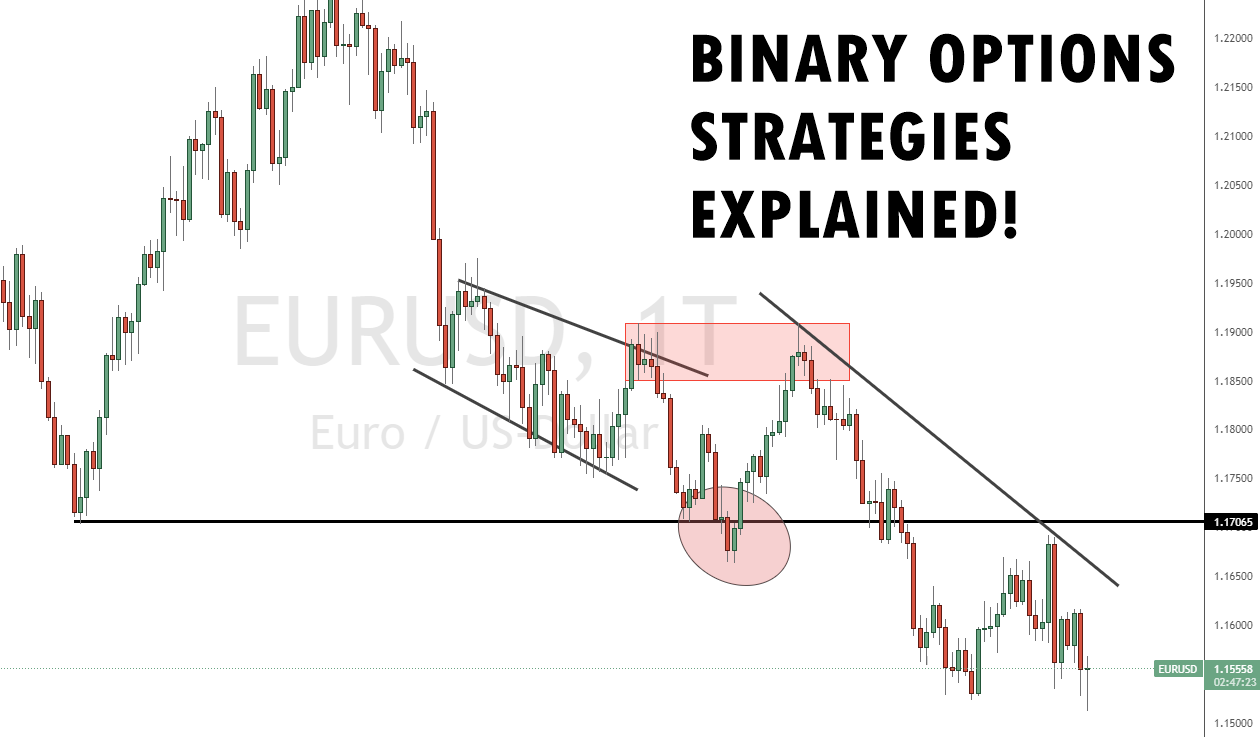
Di laman web ini, kami akan menunjukkan kepada anda 6 Strategi Pilihan Perduaan terbaik kami. Mereka telah mencapai kadar melebihi 70%. Anda boleh menggunakannya dengan mudah dalam setiap tempoh masa seperti 60 saat atau masa tamat tempoh yang lebih tinggi. Selain itu, adalah mungkin untuk menggunakan strategi Martingale untuk meningkatkan hasil anda. Yang terbaik dipanggil “Strategi Pemecahan Palsu”. Ia berfungsi pada setiap aset dan dalam setiap jangka masa. Belajar untuk berdagang dengan menguntungkan dalam beberapa saat. Lihat gambar di bawah untuk kesan pertama.
Jika anda hanya berdagang gaya perdagangan ini, ia adalah mungkin untuk membuat banyak wang. Dalam bab seterusnya, kami akan memberikan anda lebih banyak maklumat untuk menang melawan pasaran!
Senarai 6 Strategi Dagangan Pilihan Perduaan Terbaik:
- Strategi Pemecahan Palsu
- Ikuti Strategi Trend
- Strategi Pelangi
- Strategi Candlestick
- Strategi Indeks Aliran Wang
- Strategi Penyu
Satu ramalan yang salah boleh menyebabkan anda kehilangan sejumlah wang yang lumayan. Oleh itu, adalah penting untuk mewujudkan strategi binari tertentu untuk menguruskan risiko dan wang. Disebutkan di bawah adalah strategi dagangan teratas:
1. Strategi Pemecahan Palsu
Strategi False Breakout ialah cara paling tepat untuk berdagang pasaran. Pelarian dagangan tidak berfungsi dengan baik. Kami telah mengujinya berkali-kali pada masa lalu (Kami akan menunjukkan kepada anda sebab mengapa ia tidak berfungsi dengan baik di bawah). Selepas penembusan, pasaran kembali pada kebanyakan masa.
Apa yang anda perlu lakukan: adalah mencari tahap (tinggi/rendah atau sokongan/rintangan) dan tunggu sehingga pasaran menembusi tahap. Jika pasaran kembali, anda boleh pergi short (put) dan long (call).
Pemecahan Palsu: Pasaran memecahkan tahap tinggi/rendah atau sokongan/rintangan dan kembali ke tahap, dan kekal di bawah/atas tahap. Sokongan/rintangan adalah lebih daripada satu tinggi/rendah berturut-turut. Anda boleh menggunakan kaedah ini dalam mana-mana tempoh masa dan dengan mana-mana aset/pasaran. Ia adalah universal. Lihat gambar di bawah!

Lihat video kami tentang strategi binari ini:
(Amaran risiko: Modal anda boleh berisiko)
Mengapakah Strategi Binary Options ini berfungsi dengan baik?
Untuk soalan ini, adalah penting untuk mempunyai lebih banyak pengetahuan. Pada paras tinggi dan rendah adalah banyak henti rugi daripada pedagang lain di pasaran. Pedagang profesional menggunakan pengetahuan ini untuk mendapatkan kecairan yang tinggi untuk kedudukan mereka sendiri. Mereka berhenti atau membuka perdagangan dengan kecairan yang tinggi. Dalam kebanyakan kes, mereka akan memalsukan penembusan ini, atau pasaran akan bertukar kerana kedudukan tertutup.
Terdapat banyak pedagang yang akan berdagang pelarian sedemikian. Algoritma diprogramkan dan dicetuskan untuk membuat mereka kehilangan wang.
Fakta:
- Henti kerugian dicetuskan dengan penembusan
- Banyak henti rugi bermakna kecairan yang lebih tinggi
- Ilmu ini digunakan untuk membuka atau menutup kedudukan besar
- Pasaran akan berubah dalam kebanyakan kes
- Kadangkala ia adalah pemulihan yang singkat, dan kadangkala, arah aliran akan berubah sepenuhnya
Tahap manakah yang terbaik untuk berdagang?
Tinggi dan rendah baharu dan segar adalah tahap terbaik untuk strategi terbaik untuk perdagangan binari ini! Dengan beberapa tahap tertinggi berturut-turut, kemungkinan besar pasaran akan menembusi tahap ini. Cari paras tertinggi baharu dan segar. Untuk hasil terbaik, tahap harus dibuat pada hari semasa. Lihat gambar di bawah.

Tambahan pula, tahap terbaik mendapat Borang-V. Kami akan tunjukkan gambar di bawah. V-Borang dilihat dengan jelas oleh ramai peniaga lain di pasaran. Mereka meletakkan henti rugi mereka pada tahap ini. Juga, adalah mungkin untuk menukar bentuk V sebagai sokongan dan rintangan. Kami lebih suka menunggu pecahan palsu V-Borang. Ia berfungsi dengan kadar hit yang tinggi dan anda boleh membuat wang dengan mudah dengan Perdagangan Opsyen Binari.
(Amaran risiko: Modal anda boleh berisiko)

Bila hendak memilih penyertaan anda? - Untuk boneka
Pedagang berisiko membuka kedudukan secara langsung di bertentangan dengan pelarian. Pada pendapat kami, ada cara yang lebih baik untuk mendapatkan hasil yang baik. Dalam gambar di bawah, kami akan menunjukkan kepada anda entri yang tepat. Pilih tahap dalam pasaran. Jika pasaran melepasi tahap kembali, anda boleh membuka dagangan. Ia adalah semudah yang didengari. Kadangkala anda memerlukan 2-3 dagangan untuk mendapatkan keuntungan. Itulah sebabnya kita menggandakan jumlah pelaburan jika kita kehilangan perdagangan.
Maklumat tambahan: Anda boleh menunggu sehingga lilin ditutup di bawah/atas tahap pecahan untuk mendapatkan pengesahan yang lebih baik
Jangka masa yang manakah boleh saya gunakan untuk Strategi Binary Options ini?
Anda boleh menggunakan mana-mana tempoh masa untuk strategi terbaik ini untuk pilihan binari. Masa tidak penting untuk analisis anda. Hanya harga aset yang penting. Tiada peniaga profesional mengambil berat tentang masa. Anda akan melihat bahawa jangka masa yang kecil lebih sukar untuk didagangkan kerana anda perlu memberi lebih perhatian kepada pasaran. Anda perlu bertindak balas dengan lebih pantas berbanding dalam jangka masa yang lebih tinggi. Kesimpulannya, hanya harga aset yang penting.

Lihat video lain dengan contoh tepat pelarian palsu:
2. Ikut strategi trend

Ini adalah salah satu strategi perdagangan binari terbaik untuk pemula. ini strategi ikut trend boleh digunakan di mana-mana tanpa mengira jumlah dagangan atau pasaran. Pertama, anda mesti mengkaji graf perdagangan dan corak garisan. Anda mesti memerhatikan bahawa mereka biasanya pergi secara zigzag. Ini mungkin kelihatan seperti kerja yang mudah, tetapi ia memerlukan latihan.
Pertama, adalah lebih baik untuk membiasakan diri dengan graf dagangan dan arah aliran mereka pada aplikasi dagangan demo sebelum berdagang wang anda dalam pasaran masa nyata.
Sebaik sahaja anda belajar membaca corak, mudah untuk meramalkan sama ada harga aset akan naik tinggi atau rendah. Walau bagaimanapun, strategi binari terbaik ini tidak begitu boleh dipercayai untuk dagangan pendek. Untuk menggunakan strategi pilihan binari terbaik ini, anda mesti mengkaji carta dan melihat pergerakan garisan.
Jika talian naik, harga meningkat dan begitu juga sebaliknya. Jika garisan lurus mendatar, kemudian cari beberapa pilihan lain untuk berdagang wang anda.
Adalah penting untuk mempunyai pengetahuan praktikal, berlatih di tapak perdagangan demo dan mendapatkan idea yang jelas.
(Amaran risiko: Modal anda boleh berisiko)
3. Strategi pelangi

Penggunaan strategi pilihan binari yang paling tepat ini mesti dilakukan dalam kombinasi dengan strategi berita. Pertama, anda mesti tahu sifat pasaran yang anda berdagang. Kemudian, selepas mengetahui tentang trend yang sedang berlaku, anda boleh mula menggunakan strategi ini. Ini adalah strategi yang kuat yang meningkatkan peluang ramalan yang betul dan menang.
Strategi perdagangan binari terbaik ini menggunakan isyarat asas untuk membuat ramalan yang boleh dipercayai tentang harga aset.
Strategi pelangi ialah corak yang merangkumi penggunaan pelbagai purata dalam tindakan dengan tempoh yang berbeza-beza. Setiap tempoh ini dikenal pasti dengan warna yang berbeza.
Purata bergerak digunakan untuk mengenali perubahan harga. Purata bergerak dengan banyak tempoh bertindak balas dengan perlahan terhadap perubahan harga dan purata bergerak dengan beberapa tempoh bertindak balas dengan cepat.
Jika anda melihat pergerakan yang kuat dalam carta aset, purata bergerak berkemungkinan besar akan bergerak dari arah perlahan ke arah pantas dalam arah aliran masa nyata.

Purata yang bergerak paling pantas akan diletakkan paling hampir dengan harga aset, kedua terdekat akan menjadi kedua terpantas, dan ketiga paling hampir dengan harga akan menjadi purata bergerak ketiga terpantas, dan seterusnya.
Apabila anda melihat bahawa banyak purata bergerak diletakkan dalam corak seperti yang dibincangkan di atas, anda boleh mengatakan pergerakan harga yang tahan lama dalam arah yang ditentukan. Oleh itu, apabila anda menghadapi corak dan trend sedemikian, tukarkan wang anda dengan segera kerana ini adalah masa yang sesuai.
Anda boleh memilih berapa banyak purata yang anda ingin gunakan. Kebanyakan peniaga yang baik menggunakan tiga purata bergerak.
Jika purata bergerak diposisikan supaya garis terpendek berada di atas purata bergerak sederhana dan yang terpanjang berada di bawah garis sederhana atau purata bergerak. Anda mesti berdagang pada harga aset yang jatuh.
Ia bergantung kepada anda untuk menentukan bilangan purata bergerak dalam sesuatu tempoh. Oleh itu, adalah disyorkan untuk menggunakan dupleks tempoh yang anda gunakan sebelum ini dalam setiap purata bergerak.
Perubahan dalam bilangan tempoh yang digunakan dalam purata bergerak yang berbeza ini akan memberi anda nisbah yang boleh dipercayai, yang seterusnya akan memberikan anda isyarat yang tepat.
Bagi pemula, dinasihatkan untuk menggunakan nisbah 5, 10, 15, 20, dan seterusnya.
Langkah-langkah yang boleh anda ambil untuk mencapai susunan yang betul:
- Berdagang dengan segera – sebaik sahaja anda mencapai corak yang diingini atau biasa selepas purata pergerakan terakhir diposisikan, inilah masa yang sesuai untuk melabur wang anda.
- Amalkan kesabaran – jika anda ingin menguji strategi terbaik untuk pilihan binari dan elakkan semua masuk, kemudian tunggu untuk satu tempoh. Dengan cara ini, anda boleh menyemak sama ada isyarat itu membantu anda membuat ramalan yang betul atau tidak.
- Tunggu 2-3 tempoh – langkah ini memberikan anda rasa selamat, terutamanya apabila anda berdagang dengan jumlah wang yang besar dan tidak mahu mengambil risiko bergantung pada satu tempoh sahaja. Anda menunggu selama dua hingga tiga tempoh atau lebih mengikut kehendak anda.
- Luangkan masa anda untuk memahami arah aliran carta aset dan kemudian bergerak. Walau bagaimanapun, tunggu tidak lebih daripada tiga tempoh. Selepas tiga tempoh, pasaran mungkin mula berubah, dan trend baharu mungkin berlaku.
(Amaran risiko: Modal anda boleh berisiko)
4. Strategi candlestick

Steve Nison memperkenalkan strategi pembentukan candlestick binari dalam salah satu bukunya pada tahun 1991. Seorang peniaga yang baik mesti tahu membaca carta aset.
Sebaik sahaja anda memahami corak dan pergerakannya, mudah untuk anda meramalkan pergerakan aset seterusnya dalam carta. Sebagai contoh, terdapat pembentukan corak dalam carta aset yang dipanggil pembentukan candlestick. Corak yang dibentuk oleh garisan naik dan turun kelihatan seperti batang lilin.
Garis atas adalah harga tertinggi, dipanggil gunung, dan garis bawah adalah yang paling rendah, dipanggil lembah. Tidak ada satu formasi khusus dalam strategi ini, tetapi terdapat beberapa yang anda mesti pelajari untuk mengenal pasti dan membaca untuk berdagang dengan lebih baik.
Untuk menggunakan strategi perdagangan pilihan binari ini, anda mesti memerhatikan carta dan corak harga untuk seketika. Anda akan melihat beberapa pembentukan corak berulang. Kemudian anda boleh menggunakan pengetahuan dan pengalaman anda untuk meramalkan sama ada garisan itu akan naik atau turun.
(Amaran risiko: Modal anda boleh berisiko)
5. Strategi Indeks Aliran Wang

Strategi terbaik pilihan binari ini bermanfaat jika anda merancang untuk bermain dengan cepat, katakan 5 minit. Ya, strategi ini berfungsi dengan pantas. Ia pantas dan berkesan.
Sebagai seorang peniaga perdagangan pilihan binari, anda mesti sedar bahawa pasaran dagangan tidak rawak dalam jangka pendek. Satu lagi faedah strategi ini ialah ia menjimatkan banyak masa anda. Jika anda bermain dalam 5 minit, anda boleh membuat lebih banyak dagangan setiap hari.
Walau bagaimanapun, perdagangan pilihan binari jangka pendek tersebut strategi diperlukan pengurusan risiko dan analisis teknikal. Anda mesti tahu bahawa harga saham tidak berubah dalam masa 5 minit, tidak kira sama ada syarikat itu bekerja dengan baik atau teruk di pasaran. Jadi, strategi indeks aliran wang adalah menjimatkan masa tetapi juga termasuk banyak risiko.
Satu-satunya perkara yang mengubah harga aset dalam tempoh yang singkat ialah permintaan dan penawaran. Kedua-dua faktor ini menentukan sama ada harga aset akan naik atau turun dalam tempoh yang ringkas.
Untuk menguasai strategi ini dan membuat wang setiap 5 minit dengan Pilihan Perduaan, anda mesti mempelajari analisis teknikal. Ini akan membantu anda dalam memahami sama ada peniaga lain menjual atau membeli. Sebaik sahaja anda memahami perkara ini, mudah untuk menggunakan strategi MFI dengan penunjuk indeks aliran wang.
Penunjuk indeks MFI – penunjuk memberitahu anda nisbah aset yang dijual kepada bilangan aset yang dibeli. Nilai biasanya antara 0-100.
Marilah kita memahami cara penunjuk indeks aliran wang berfungsi:
- Angka 0 – menunjukkan bahawa ramai pedagang aktif merancang untuk menjual aset tersebut.
- Angka 50 – menunjukkan bahawa bilangan pedagang aktif yang sama ingin membeli dan menjual aset tersebut.
- Angka 100 – menunjukkan bahawa semua pedagang yang aktif di platform ingin membeli aset tersebut.
Sekarang setelah anda memahami hubungan antara nisbah penunjuk MFI dan peniaga yang merancang untuk membeli atau menjual aset, anda akan menjadi mudah untuk memilih satu pilihan dan menjamin wang anda. Selain itu, anda boleh menganggarkan pergerakan harga aset dengan mudah selepas memahami permintaan dan penawaran.
Dengan kata yang lebih mudah, jika bilangan peniaga yang membeli aset adalah lebih besar daripada bilangan peniaga yang menjual aset yang sama. Akan ada lebih sedikit peniaga untuk memaksa harga aset naik. Akibatnya, permintaan dan harga kedua-duanya akan turun.
Dengan cara yang sama, jika bilangan peniaga yang menjual aset lebih besar daripada bilangan peniaga yang membelinya, bekalan akan berkurangan, dan harga akan meningkat.
Disebutkan di bawah ialah cara anda boleh menggunakan indeks MFL untuk ramalan tepat anda yang seterusnya:
- Jika indeks aliran wang lebih daripada 80. Ini bermakna ramai peniaga membeli aset tersebut, dan harga mungkin jatuh.
- Jika indeks aliran wang kurang daripada 20. Ini bermakna ramai peniaga menjual aset tersebut, dan harga mungkin akan meningkat.
Strategi terbaik untuk berdagang pilihan binari ini berfungsi paling baik untuk tempoh yang singkat. Pedagang biasanya menggunakan strategi ini untuk bermain pertaruhan 5 minit. Dalam jangka panjang, adalah sukar untuk meramalkan proses melalui strategi ini kerana ia melampau. Jadi, elakkan menggunakan strategi ini untuk dagangan jangka panjang anda.
(Amaran risiko: Modal anda boleh berisiko)
6. Strategi Penyu

Ini adalah salah satu strategi pilihan binari terbaik di kalangan pedagang. Seperti namanya, strategi ini menggunakan pergerakan harga aset dalam dua puluh hari yang lalu. Kemudian gunakan data ini untuk meramal hit seterusnya; ia mungkin tinggi atau rendah. Strategi ini memberi anda dua isyarat:
- Isyarat beli – apabila pergerakan harga semasa lebih tinggi daripada bar/garisan 20 hari lepas.
- Isyarat jual – apabila pergerakan harga semasa lebih rendah daripada bar/garisan 20 hari yang lalu.
Ini adalah salah satu strategi perdagangan pilihan binari terbaik dan ia boleh digunakan dengan mudah oleh pemula. Walau bagaimanapun, keputusan strategi penyu telah bercampur-campur. Strategi dagangan membantu pedagang dalam mengenal pasti isyarat; tiada satu pun daripada mereka menjanjikan 100% tepat.
Apakah strategi Pilihan Perduaan?
Strategi Pilihan Perduaan ialah kaedah dagangan yang digunakan untuk meramalkan pergerakan harga aset asas tertentu dan menentukan sama ada untuk membeli atau menjual pilihan binari.
Strategi Pilihan Perduaan harus mengikut peraturan ketat pelan dagangan anda. Strategi boleh dilaraskan kepada mana-mana tempoh masa, pasaran atau platform dagangan yang menawarkan dagangan binari. Tanpa strategi Pilihan Perduaan anda berdagang buta dalam pasaran dan keuntungan dan kerugian anda dijana secara rawak.
Mengapa anda memerlukan strategi Binary Options?
Strategi Pilihan Perduaan boleh menjadi kaedah yang berbeza untuk berdagang pasaran. Pertama sekali, Strategi Pilihan Perduaan tidak semestinya sukar. Ia adalah mungkin untuk membuat wang dengan idea dan kaedah yang mudah. Oleh itu adalah penting untuk menggunakan peraturan yang ketat untuk berdagang pasaran. Kesilapan yang paling biasa ialah tidak mematuhi peraturan anda sendiri! Di samping itu, strategi yang baik mengurangkan perdagangan emosi dan tidak rasional.
Kebanyakan peniaga kehilangan wang mereka kerana mereka berdagang tanpa kaedah dan strategi yang terbukti. Pedagang maju tahu cara pasaran berfungsi, dan mereka banyak mempraktikkan kaedah mereka sendiri. Anda perlu belajar dan mendapatkan pengetahuan yang lebih tinggi tentang pasaran. Daripada pengalaman kami, bukan mudah untuk belajar berdagang dengan jayanya dalam masa yang singkat. Dalam artikel berikut, kami akan memberikan anda peraturan yang ketat untuk berdagang pasaran dan kami akan menunjukkan kepada anda bagaimana strategi berfungsi dengan mudah dan berjaya.
Sebab untuk menggunakan strategi perdagangan Pilihan Perduaan:
- Melaksanakan tindakan tanpa perancangan atau strategi yang betul adalah tertakluk kepada kegagalan. Oleh itu, adalah penting untuk membuat strategi sebelum berdagang wang anda di mana-mana platform.
- Ia adalah wang sebenar yang anda berurusan. Untuk menjadi peniaga yang berjaya, anda mesti tahu tempat anda meletakkan wang anda.
- Jangan sekali-kali menganggap perdagangan sebagai perjudian semata-mata jika anda berusaha untuk menjadi peniaga yang baik. Jangan bergantung pada tekaan. Dengan cara ini, anda hanya akan kehilangan wang anda.
- Menggunakan strategi memberi anda isyarat kukuh tentang pergerakan harga aset. Walau bagaimanapun, anda hanya boleh menggunakan situasi untuk membuat keuntungan besar jika anda memahami arah aliran dan meramalkan dengan betul.
- Ia menyelamatkan anda daripada membuat keputusan yang impulsif dan emosi.
- Sebaik sahaja anda membangunkan strategi terbaik untuk pilihan binari yang sesuai untuk anda, anda boleh menguasai dan mengubah suainya untuk membuat keuntungan jangka panjang.
- Menggunakan strategi pengurusan wang untuk menentukan jumlah wang yang anda akan laburkan dalam perdagangan boleh menyelamatkan anda daripada kehilangan wang anda secara tidak bertanggungjawab. Oleh kerana ketamakan dan rasa bersalah dengan mudah boleh memanipulasi anda untuk mengambil tindakan spontan.
Asas strategi perdagangan Binary Options yang berjaya
Sebelum melangkah ke lapangan, anda mesti mengetahui dua parameter asas strategi perdagangan pilihan binari – jumlah dagangan dan isyarat. Marilah kita memahami kedua-dua parameter ini secara terperinci:
#1 Isyarat
Isyarat pada asasnya adalah pergerakan dalam pasaran atau petunjuk sama ada harga akan naik atau turun. Ia lebih seperti naluri selepas memerhatikan trend yang berlaku di sekeliling anda. Isyarat membantu anda mengenal pasti langkah seterusnya dengan lebih lanjut. Jelas sekali, ia membantu anda meramalkan sama ada harga akan naik atau turun.
Terdapat cara tertentu yang anda boleh mengenal pasti isyarat. Berikut adalah beberapa cara:
- Kekal dikemas kini
Perdagangan adalah berkaitan dengan perniagaan dan pasaran. Jadi, untuk pandai berdagang, anda mesti mempunyai pengetahuan yang baik tentang saham atau pasaran saham, berita industri, dan maklumat yang diberikan kepada orang ramai oleh CEO. Semua ini boleh membantu anda meramalkan sama ada harga sumber akan naik atau turun.
- Tinjauan teknikal
Ini ialah kaedah di mana anda mengetepikan berita pasaran dan melihat dengan teliti pada graf dagangan. Ia adalah pendekatan yang lebih berpusat. Anda membaca graf dengan teliti dan menganalisis peristiwa masa lalu untuk meramalkan masa depan.
Ia rumit tetapi lebih dipercayai. Anda tidak perlu pergi semua-in; terdapat banyak aplikasi dagangan demo tersedia dalam talian di mana anda boleh berlatih dan meningkatkan kemahiran meramal anda. Setelah otak anda terbiasa dengan corak dagangan, ia akan mudah untuk memahami arah aliran harga naik atau turun.
#2 Jumlah pelaburan
Adalah penting untuk menentukan jumlah wang yang anda akan berdagang. Menjadi impulsif atau salah urus wang hanya akan mengakibatkan kerugian. Membangunkan a strategi untuk menguruskan wang anda untuk mengurangkan risiko melalui Binary Options. Berikut ialah dua strategi pengurusan wang yang paling banyak digunakan dan boleh dipercayai - pendekatan berdasarkan peratusan dan martingale.
- Pendekatan berasaskan peratusan
Dalam kaedah ini, anda memutuskan berapa peratusan modal anda yang anda ingin berdagang. Untuk pemula, kami mengesyorkan bermula dengan 1% atau 2%. Sebagai contoh, anda mempunyai $ 50,000 dalam akaun bank anda. Jadi, anda memutuskan untuk berdagang 1% daripadanya, iaitu $ 500. Ini ialah cara yang selamat untuk mengurus wang anda dan mengurangkan potensi risiko.
Pendekatan ini agak rumit dan berisiko jika anda tidak berpengalaman. Tetapi adalah baik untuk membiasakan diri dengan semua pendekatan yang mungkin. Di sini anda menggandakan dagangan pagi
Menguji jika strategi perdagangan binari berfungsi untuk anda
Jadi, apakah strategi terbaik binari? Terdapat sejumlah besar variasi yang anda akan temui di internet. Setiap daripada mereka akan kelihatan boleh dilaksanakan sehingga anda mengujinya. Pedagang yang berbeza melihat isyarat secara berbeza. Mengenal pasti strategi yang paling sesuai untuk anda akan membantu anda menjana wang dalam jangka masa panjang.
Tiada apl atau orang boleh memberitahu anda strategi pilihan binari yang paling sesuai untuk anda. Ia adalah kerja seorang peniaga untuk menguji strategi perdagangan yang berbeza dan membentuknya dalam caranya untuk memanfaatkannya sepenuhnya. Perdagangan binari memerlukan ramalan yang tepat. Ia menuntut penguasaan terhadap strategi untuk menang. Penggunaan mana-mana strategi atau isyarat campuran yang salah akhirnya akan menyebabkan anda kehilangan wang.
Elakkan menggunakan wang sebenar untuk menguji strategi baharu. Di samping itu, pastikan anda menetapkan had dan mempunyai strategi untuk menguruskan wang anda.
Cari jangka masa yang sesuai untuk strategi pilihan binari:
Jangka masa manakah yang terbaik untuk berdagang Pilihan Perduaan dengan strategi? – Broker menawarkan anda untuk berdagang 30 saat, 60 saat, 5 minit, atau bahkan 24 jam masa tamat pada perdagangan binari. Daripada pengalaman kami, anda boleh menggunakan strategi yang dibincangkan dalam setiap jangka masa yang anda mahukan. Ia sentiasa sama, jangka masa tidak penting.

Tetapi kami boleh mengesyorkan untuk menjauhkan diri daripada jangka masa 30 saat atau 60 saat jika anda seorang pemula kerana anda memerlukan kemahiran yang sangat tinggi untuk melakukan pelaksanaan perdagangan yang pantas.
Pengurusan wang untuk kejayaan yang terbaik
Pengurusan Wang adalah milik setiap Strategi Binary Options. Tanpa pengurusan wang yang betul, anda akan kehilangan segala-galanya. Kebanyakan peniaga membuat kesilapan ini. Kami secara peribadi lebih suka mempertaruhkan 1 – 5% baki akaun dagangan kami dalam satu Binary Options. Jadi anda boleh kehilangan beberapa dagangan tanpa memusnahkan akaun anda sepenuhnya. Pengurusan wang bergantung kepada peniaga juga. Sesetengah peniaga sangat agresif dan mengambil banyak wang untuk melabur. Pada akhirnya, anda perlu memutuskan sendiri berapa banyak wang yang anda mahu risiko.
Sesetengah peniaga menggunakan 10% atau lebih baki akaun untuk berdagang. Contohnya, jika anda mendapat 4 dagangan yang rugi (ini berlaku) berturut-turut, baki akaun anda adalah tolak 40%. Pada pendapat kami, adalah tidak waras untuk menggunakan risiko ini.
Kebanyakan peniaga profesional menggunakan risiko 0.5 – 1,5% portfolio mereka untuk satu dagangan. Dari pengalaman saya, anda akan mengalami emosi yang sukar dengan kehilangan sejumlah besar wang dalam masa yang singkat atau beberapa dagangan.
Pertama sekali, ia kelihatan seperti proses yang sukar untuk melabur hanya 1% atau kurang daripada portfolio anda, tetapi dengan strategi dagangan yang mantap dan berterusan, anda akan memperoleh banyak wang pada masa hadapan. Sebagai contoh, jika anda membuat keuntungan sebanyak 2% setiap hari, akaun akan berkembang sangat tinggi dalam beberapa minggu.
Martingale untuk Strategi Binary Options Breakout Palsu
Untuk hasil yang lebih baik, anda boleh menggunakan yang popular “Strategi Martingale”. Jika anda kehilangan perdagangan anda, anda boleh gandakan pelaburan anda atau gunakan lebih daripada 2,3x pelaburan terakhir dalam perdagangan seterusnya. Ini sangat berisiko, tetapi dengan strategi yang berjaya, ini adalah cara yang baik untuk digunakan. Pada pendapat saya, hanya peniaga yang berpengalaman harus menggunakan "Martingale".
Martingale boleh meletupkan akaun anda dalam beberapa dagangan. Kami hanya menggunakannya apabila kami berasa sangat selamat untuk perdagangan seterusnya dan kami mengesyorkannya.
- Gunakan pengurusan wang yang bijak (kami lebih suka mengambil risiko 1-5% setiap dagangan)
- Martingale ialah cara yang baik untuk Pedagang berpengalaman (gandakan jumlah dagangan jika anda kalah)
Perhatian kepada Berita Pasaran
Satu lagi titik perdagangan yang berjaya ialah berita ekonomi pasaran (gambar di bawah). Ramai peniaga menggunakan berita ekonomi ini untuk berdagang pasaran. Pada pendapat kami, ia seperti berjudi kerana anda tidak tahu keputusan berita tersebut. Di samping itu, anda terlalu lambat untuk bertindak balas dengan cepat apabila berita itu muncul. Pesanan dicetuskan dalam kurang sen 0,01 saat. Terdapat program dagangan automatik yang lebih pantas daripada anda!
Kesimpulannya, adalah bukan idea yang baik untuk memperdagangkan berita ekonomi. Nasihat saya kepada anda: Berhenti berdagang 10 minit sebelum dan selepas berita. Kemeruapan adalah sangat tinggi dan dalam kebanyakan kes, pasaran akan melompat terus ke atas skrin anda. Pasaran tidak mempedulikan angka kerana ia sudah ditetapkan harga.
Kami menggunakan berita ekonomi www.investing.com. Anda akan mendapat berita yang betul 0.1 saat selepas ia dikeluarkan.

Bermula – Gunakan Broker Binari yang baik untuk strategi anda
Dalam jadual di bawah, anda akan menemui Broker Binary Options yang terbaik. Adalah sangat penting untuk menggunakan broker dengan perisian carta yang baik. Anda perlu menganalisis candlestick/carta untuk breakout palsu. Tidak berguna untuk berdagang strategi yang berjaya untuk broker yang buruk kerana mungkin mereka tidak membayar keuntungan anda. Kami menguji Broker Pilihan Perduaan terbaik dan mengesyorkannya di laman web kami.
Awak boleh buat akaun demo untuk mempraktikkan kaedah baru berdagang pasaran ini. Broker yang disyorkan kami menawarkan anda akaun percuma dan tanpa had. Syaratnya adalah sama seperti dalam mod wang sebenar.
Satu lagi perkara yang berkaitan ialah perisian dagangan untuk pelaksanaan dagangan anda. Anda harus menganalisis carta dengan cara terbaik yang anda boleh. Gunakan candlestick- atau carta garis. Kami mengesyorkan versi candlestick. Alat lukisan ditawarkan oleh platform dan anda boleh bermula dalam beberapa saat.
Fakta untuk broker yang baik:
- peraturan
- Akaun demo percuma
- Keuntungan aset yang tinggi
- Platform dagangan yang fleksibel
- Perkhidmatan yang baik dan sokongan pelanggan
Broker di bawah memberi anda hasil tertinggi dan platform yang paling berfungsi untuk dagangan anda:
100+ Pasaran
- Min. deposit $10
- tunjuk cara $10,000
- Platform profesional
- Keuntungan tinggi sehingga 95%
- Pengeluaran cepat
- Isyarat
100+ Pasaran
- Menerima pelanggan antarabangsa
- Bayaran tinggi 95%+
- Platform profesional
- Deposit cepat
- Perdagangan Sosial
- Bonus percuma
300+ Pasaran
- Deposit minimum $10
- Akaun demo percuma
- Pulangan tinggi sehingga 100% (sekiranya ramalan yang betul)
- Platform ini mudah digunakan
- Sokongan 24/7
100+ Pasaran
- Min. deposit $10
- tunjuk cara $10,000
- Platform profesional
- Keuntungan tinggi sehingga 95%
- Pengeluaran cepat
- Isyarat
daripada $10
(Amaran risiko: Dagangan adalah berisiko)
100+ Pasaran
- Menerima pelanggan antarabangsa
- Bayaran tinggi 95%+
- Platform profesional
- Deposit cepat
- Perdagangan Sosial
- Bonus percuma
daripada $50
(Amaran risiko: Dagangan adalah berisiko)
300+ Pasaran
- Deposit minimum $10
- Akaun demo percuma
- Pulangan tinggi sehingga 100% (sekiranya ramalan yang betul)
- Platform ini mudah digunakan
- Sokongan 24/7
daripada $10
(Amaran risiko: Modal anda mungkin berisiko)
Kesimpulan daripada Strategi Binary Options terbaik:
Untuk berjaya dalam perdagangan pilihan binari, dalam jangka masa panjang, anda mesti mengamalkan strategi berulang kali. Bersama-sama dengan menggunakan strategi, anda mesti mempunyai kesabaran dan mengelakkan daripada mengambil tindakan impulsif. Menggunakan mana-mana strategi untuk satu masa tidak akan membawa keuntungan kepada anda. Menguji, mencuba dan mengulangi adalah satu-satunya cara untuk menguasai taktik perdagangan.
Jangan berhenti strategi dan pilih yang baru setiap kali anda mengalami kerugian. Ini hanya akan mengelirukan anda, dan anda tidak akan dapat memanfaatkan satu strategi yang terbaik.
Sebaliknya, berpegang pada satu strategi dan pelajari masa yang sesuai untuk menggunakannya. Ia juga penting untuk mengetahui masa apabila anda mesti mengelak daripada menggunakan strategi tertentu. Walau bagaimanapun, jika strategi anda tidak berfungsi, anda mesti mempertimbangkannya semula dan membuat yang baharu. Adalah baik untuk mengambil nasihat pakar semasa membuat strategi binari.
Sekarang setelah anda membaca beberapa strategi perdagangan pilihan binari terbaik, cari strategi yang anda fahami dengan baik dan ujinya hari ini. Kemudian, mula bertindak dan mula menjana wang hari ini!
(Amaran risiko: Modal anda boleh berisiko)
Soalan lazim:
Apakah strategi perdagangan Binary Options yang terbaik?
Tiada strategi khusus yang boleh membuktikan yang terbaik untuk semua pedagang di luar sana. Strategi yang berbeza berfungsi untuk pedagang yang berbeza. Oleh itu, anda mesti mencuba dan menguji pelbagai strategi untuk mengetahui perkara yang sesuai untuk anda. Walau bagaimanapun, mempunyai pengetahuan yang baik tentang pasaran dan mempelajari analisis teknikal akan membantu anda berjaya.
Apakah jumlah minimum yang diperlukan untuk berdagang Binary Options?
Dari mana datangnya wang keuntungan?
Tiada sumber wang luaran dalam platform dagangan binari. Wang sedang diputarkan. Sebagai contoh, dua peniaga melabur sejumlah $100. Seorang peniaga menang manakala seorang lagi kalah.
Wang yang hilang oleh pedagang itu akan dipindahkan kepada yang menang, bergantung pada peratusan keuntungan yang diberikan oleh broker kepada pedagangnya. Beberapa peratusan wang yang hilang akan pergi ke broker.
Apakah jumlah maksimum yang boleh diperolehi oleh Binary Options?
Jawapan kepada soalan ini bergantung pada jumlah wang yang didagangkan. Sebagai contoh, seorang peniaga melabur $1000, dan peratusan keuntungan yang disediakan oleh broker ialah 60%. Dalam kes ini, kemenangan akan memberi anda $600 tambahan.
Secara keseluruhan, anda akan mempunyai $1600. Walau bagaimanapun, jika anda gagal, anda akan kehilangan semua wang anda, iaitu, $1000. Tiada jumlah maksimum tetap yang boleh diperoleh melalui pilihan perdagangan. Ia bergantung pada jumlah wang yang didagangkan dan jumlah kemenangan.
Adakah strategi perdagangan Binary Options berfungsi?
Strategi perdagangan binari tidak boleh menjanjikan kejayaan 100% kepada anda. Memandangkan strategi dagangan hanya memberi anda isyarat untuk meramalkan langkah seterusnya. Strategi perdagangan tidak betul-betul memberitahu anda sama ada harga aset akan naik tinggi atau jatuh. Walau bagaimanapun, amalan dan pengetahuan yang baik tentang aset akan meningkatkan peluang anda untuk menang.
Lihat strategi dagangan saya yang lain di sini:
- Corak ABCD untuk Binary Options menjelaskan: Bagaimana untuk berdagang corak carta
- Julat Benar Purata: Bagaimana untuk menggunakan penunjuk ATR dengan Binary Options
- Strategi dagangan penunjuk MACD terbaik untuk Pilihan Perduaan
- Strategi penunjuk ATR Binary Options
- Strategi perdagangan Bollinger Band Binary Options
- Strategi pelarian Binary Options
- Carta Candlestick Binary Options – Corak & strategi terbaik
- Strategi perdagangan penunjuk CCI Binary Options
- Strategi pengkompaunan Pilihan Perduaan: Bolehkah anda menjadi Jutawan?
- Strategi pekali korelasi Binary Options
- Pilihan binari menggandakan strategi
- Strategi lindung nilai Binary Options: Bagaimana untuk menjamin keuntungan anda
- Strategi perdagangan Saluran Keltner Binary Options
- Tutorial strategi carta baris Binary Options
- Strategi perdagangan pukulan panjang Binary Options
- Strategi tarikan pasaran Binary Options
- Strategi Martingale Binary Options menjelaskan
- Strategi pengurusan wang Binary Options menjelaskan
- Perduaan Pilihan strategi ramalan lilin seterusnya
- Strategi perdagangan julat Binary Options menjelaskan
- Strategi piramid terbalik Binary Options
- Strategi perdagangan pembalikan arah aliran Opsyen Binari
- Strategi perdagangan trendline Pilihan Perduaan menjelaskan
- Strategi risiko sifar Binary Options: Adakah itu mungkin?
- Membeli penurunan dengan Binary Options - Strategi perdagangan dijelaskan
- Strategi perdagangan pengeluaran modal untuk Binary Options
- Strategi perdagangan Binary Options EUR/USD
- Strategi corak kepala dan bahu dengan Binary Options
- Bagaimana untuk berdagang Binary Options dengan strategi tindakan harga?
- Bagaimana untuk berdagang Corak Rama-rama dengan Binary Options
- Bagaimana untuk berdagang pecahan palsu dengan Binary Options
- Bagaimana untuk berdagang yang lebih tinggi dengan pilihan binari
- Bagaimana untuk berdagang tinggi rendah dan rendah lebih tinggi dengan Binary Options
- Bagaimana untuk berdagang rendah rendah dengan Binary Options
- Bagaimana untuk menggunakan corak harmonik untuk berdagang Binary Options?
- Bagaimana untuk menggunakan Penjejakan Semula Fibonacci untuk Binary Options – Strategi
- Berbilang strategi analisis rangka masa dengan Binary Options
- Strategi dagangan pelarian julat terbuka untuk Binary Options
- Strategi mata pangsi untuk perdagangan binari
- Tutorial penunjuk Kadar Perubahan Perdagangan Opsyen Binari – Strategi
- Strategi perdagangan sokongan dan rintangan untuk Binary Options
- Strategi Pilihan Perduaan 5 minit terbaik secara terperinci
- Corak cawan dan pemegang dalam perdagangan Pilihan Perduaan
- Binary Options Dagangan pada hari gaji Bukan Ladang